OHC COVID-19
Antigen Self Test
The OHC COVID-19 Antigen Self Test, a high quality test you can trust.
91% relative sensitivity and 99% relative specificity*
Prevent your loved ones from exposure to the virus with the accuracy of the OHC COVID-19 Antigen Self Test.
OHC continues to conduct studies for SARS-CoV-2 as new variants continue to emerge so that we can provide high-quality testing for you and your family.
Using the easy nasal swab test, you can self-collect samples with highly accurate and reliable results you can expect in just 15 minutes.
Children starting at the age of 14 can self test. Children from ages 2 to 13 require the help of an adult.
Feel safe and confident whether or not you have symptoms of COVID-19.
The OHC COVID-19 Antigen Self Test detects both Omicron and Delta variants.
*Clinical Data shows, OHC COVID-19 Antigen Self Test showed a relative sensitivity of 91% ( 95% CI: 82.8 to 95.6%) at high viral loads (less than a cycle threshold (Ct)-value of 30) and relative specificity of 99% (95% CI: 95.2 to 99.6%).
Kit Contents
Here's what you will find inside your kit.
-

Cassette
-

Sterile
nasal swab -

Extraction
buffer tube -

Tube
Filter Cap -

User Manual
Quick guide -

Box
(Tube holder)
INSTRUCTIONS FOR USE (IFU)
Prepare to Perform the Test
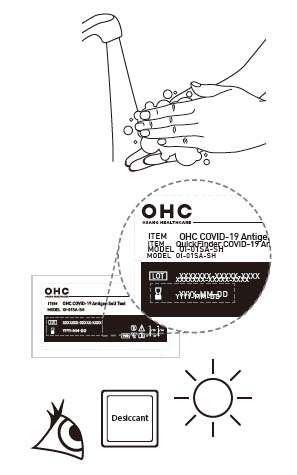
1. Bring test kit to room temperature (15-30oC / 59-86oF). **Before washing your hands, please prepare by blowing your nose.**
2. Wash your hands with soap and water, or use hand sanitizer before performing the test. Make sure you rinse thoroughly and your hands are dry before starting.
3. Check test expiration date on the back of the foil. Do not use if the expiry date has been passed.
4. Open the pouch and remove the test device from the foil pouch. Ensure the desiccant contains only white and yellow beads.
Note: If green beads are present, use a new test device.
5. Place the test device on a flat surface
Seven Easy Steps to Run a Test
STEP 1: OPEN TUBE &
PLACE TUBE IN TUBE HOLDER
Open the pouch that contains the extraction buffer tube & filter cap.
Open the seal of the tube carefully without spilling the liquid inside the tube.
Punch a hole in the box to hold the tube.
If any liquid spills, do not use the tube.
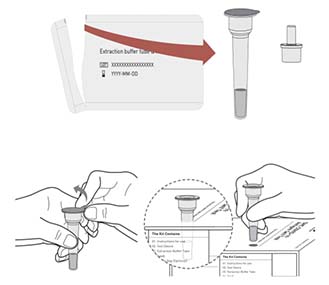
STEP 2: OPEN SWAB
Remove the swab from the packaging.
Ensure that you only touch the handle of the swab and NOT the soft pad on the tip.
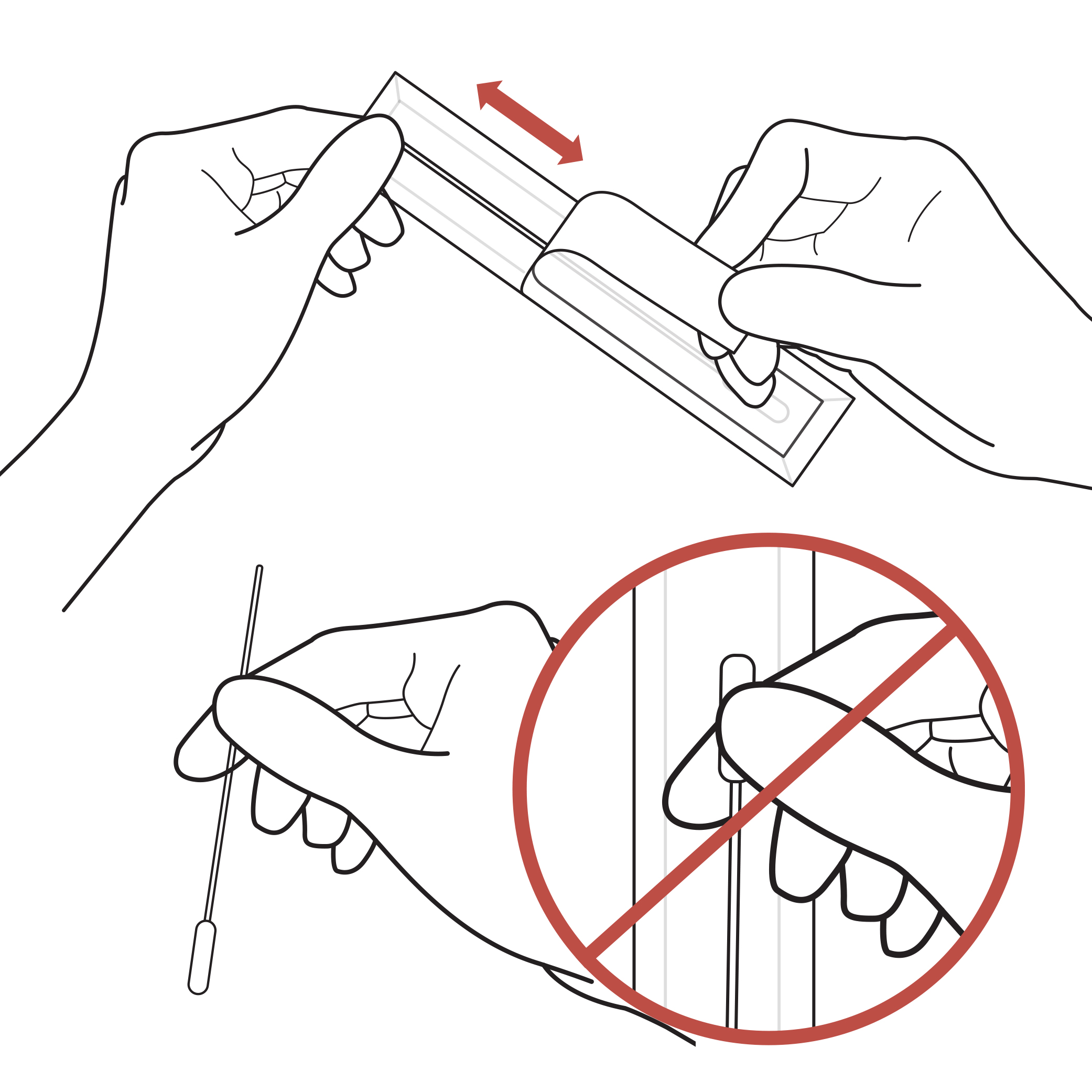
STEP 3: COLLECTION THE SAMPLE
Holding the stick end of the swab, gently insert the foam end of the swab into the nostril approximately ½ to ¾ of an inch.
Do not insert the swab any further if you feel resistance.
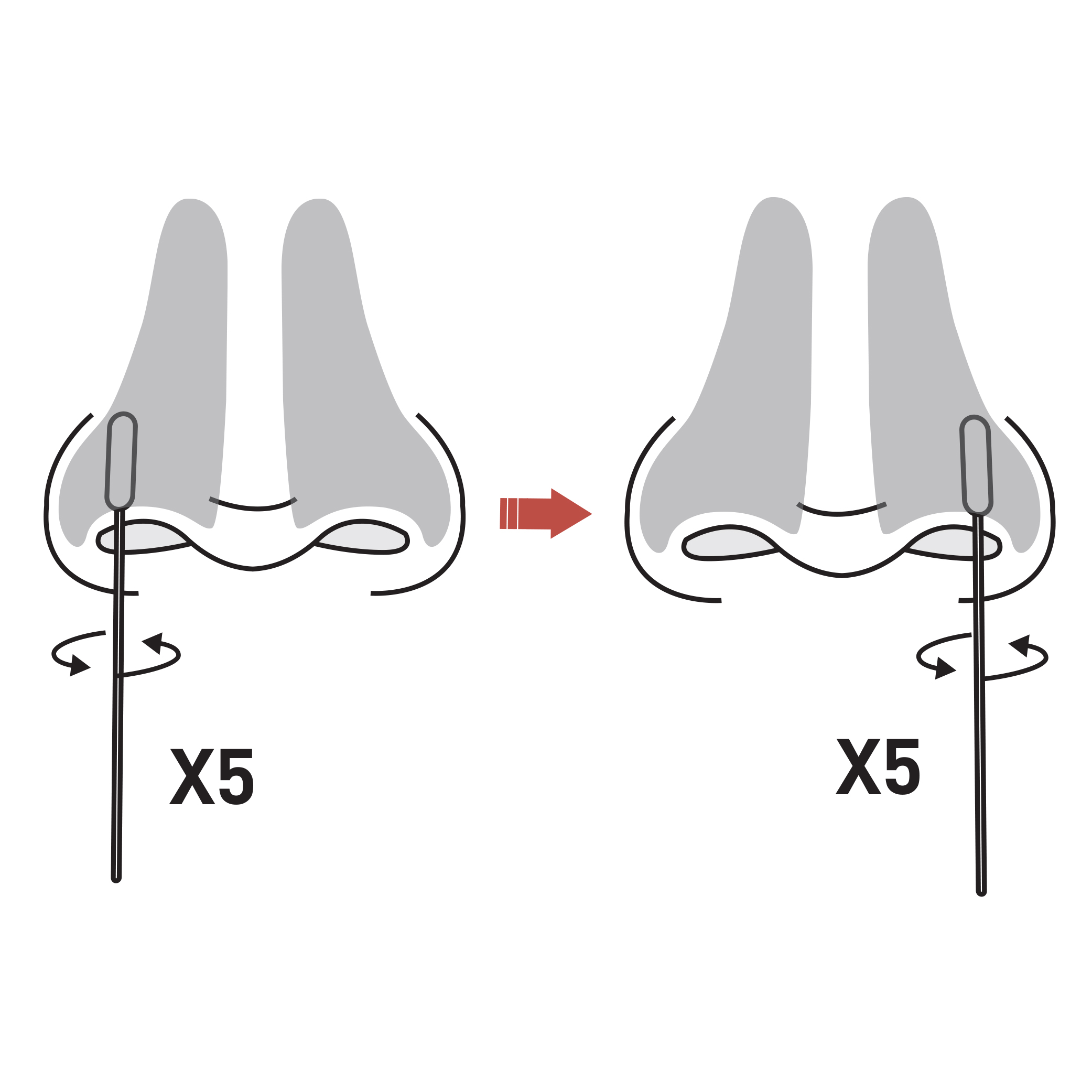
**Swab Both Nostrils**
Firmly and slowly rotate the swab at least 5 times, brushing against the inside walls of the nostril at least 5 times for a total of 15 seconds.
**Do not just spin the swab.**
Gently remove the swab, and using the same swab, repeat in the second nostril with the same end of the swab.
NOTE: When swabbing others, please wear a face mask. With children, the maximum depth of insertion into the nostril may be less than 3/4 of an inch, and you may need to have a second person to hold the child’s head while swabbing.
WARNING! Inaccurate test results may occur if the nasal swab specimen is not properly collected.
STEP 4: REMOVE THE SWAB &
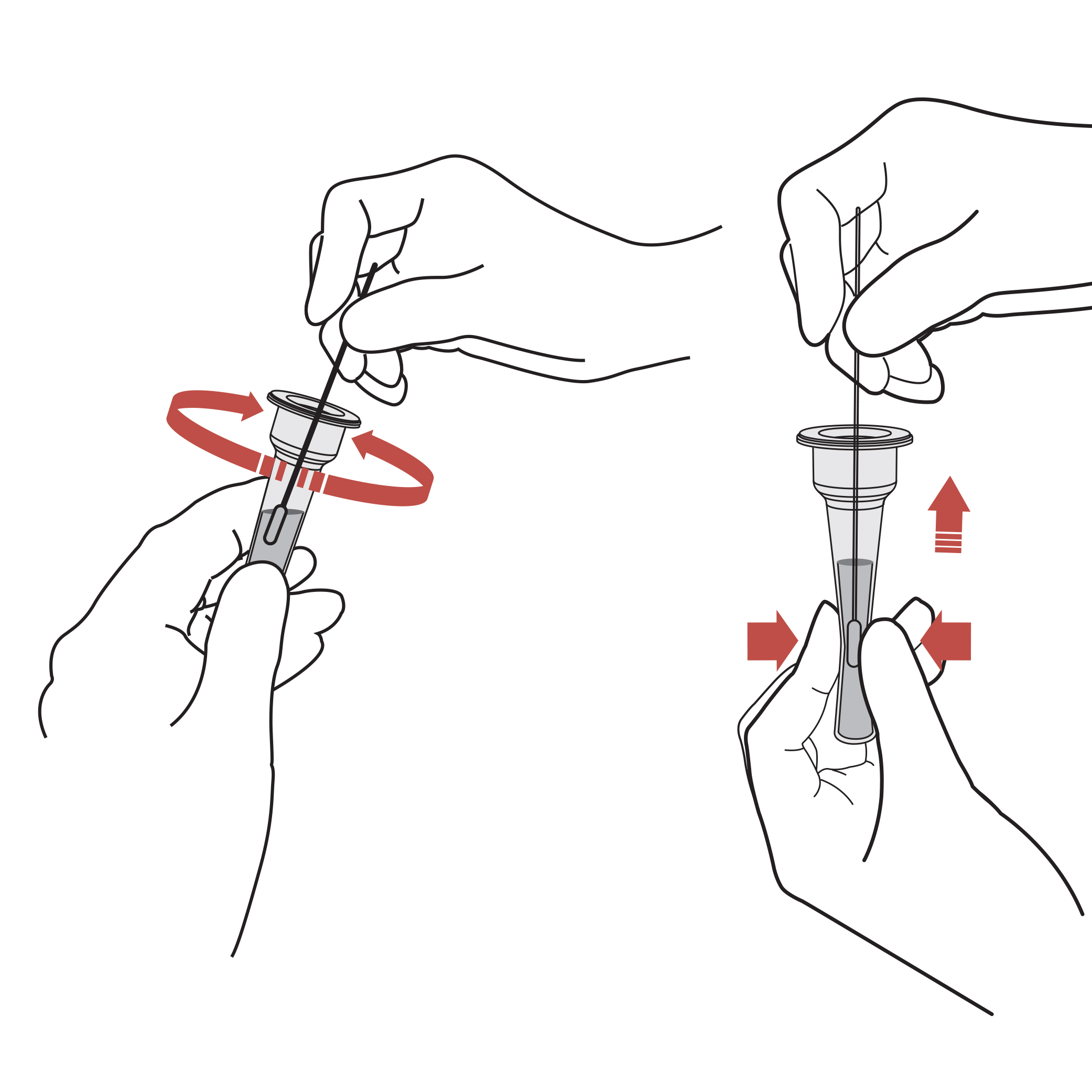
PLACE IT INTO THE TUBE & MIX
Directly Insert the sterile swab taken from the nostril into the extraction buffer tube and stir it more than 10 times. Take out the swab from the extraction buffer tube by squeezing and applying pressure on both sides of the tube.
WARNING! Failure to squeeze the tube can lead to incorrect results due to excess buffer in the swab.
WARNING! The sample should be mixed into the buffer immediately, but no more than an 1 hour after collecting the sample.
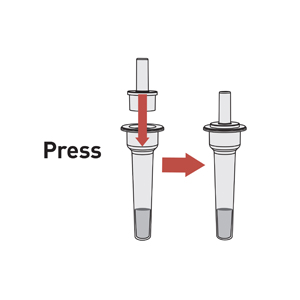
STEP 5: DISPOSE THE SWAB & SEAL THE TUBE
Dispose of the swab and seal the tube securely with the nozzle cap.
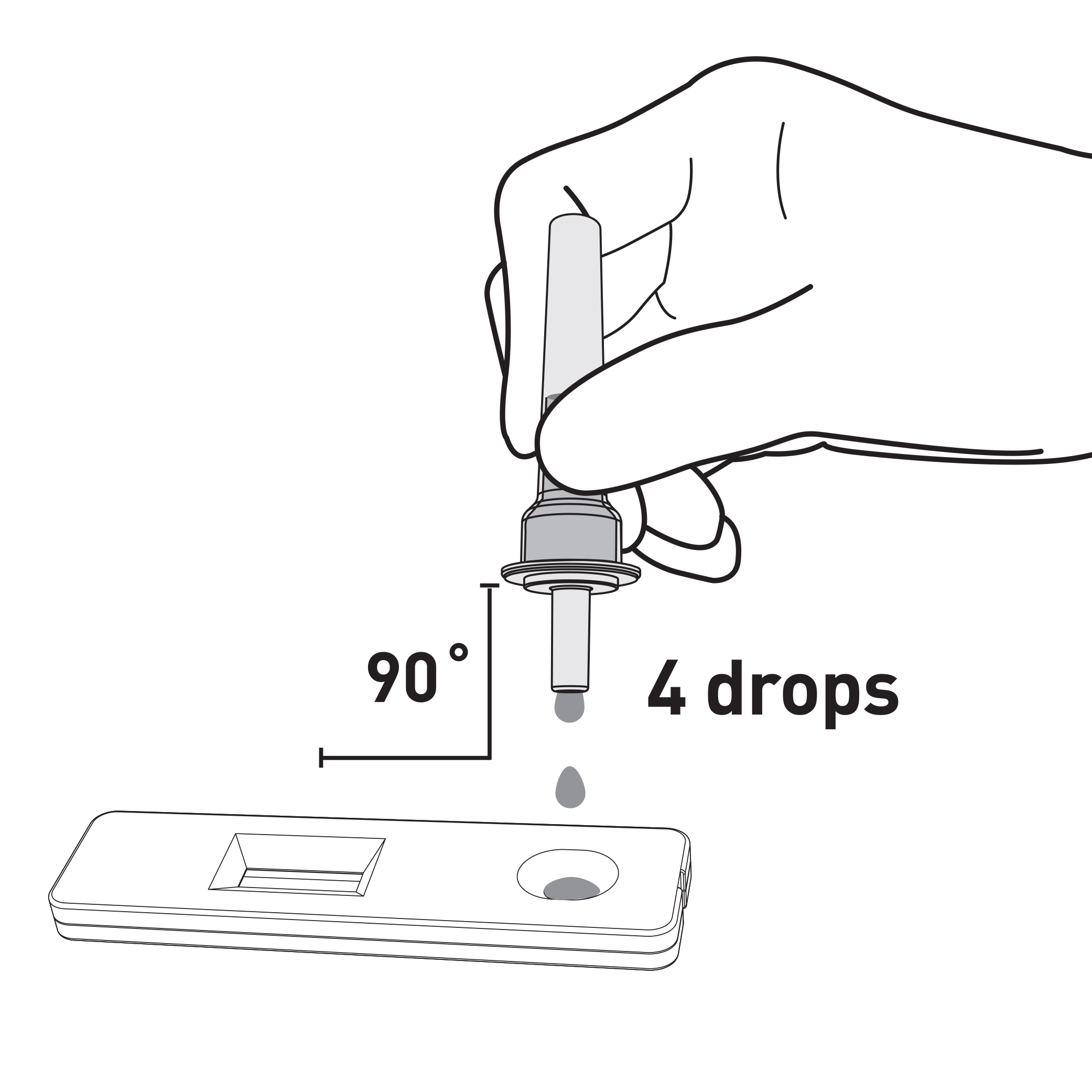
STEP 6: ADD 4 DROPS
INTO THE CASSETTE SAMPLE WELLDROPS INTO THE CASSETTE SAMPLE WELL
Hold the tube uprights above the sample well. Drop 4 drops onto the sample well.
**Do not apply the liquid in the rectangular result window.**
WARNING! Adding more or less than 4 drops of solution into the sample well may result in incorrect results.
STEP 7:
Set the timer and read the test result at 15 minutes.
Do not read the result after 20 minutes.
Read test result at 15 minutes DO NOT read after 20 minutes.
WARNING! Do not move or lift the test device during this time.
After the test is completed, dispose of used materials in household trash. Do not flush or pour test liquids down a drain.

READ & INTERPRET THE RESULTS
WARNING! Inaccurate test interpretations may occur if results are read before 15 minutes or after 20 minutes.
Look at the result window and locate the letters C and T on the side of the window. A pink/purple line should always appear at the C position; this is a control line and signals that the test is working properly.
Report your test result(s) at MakeMyTestCount.Org – this voluntary and anonymous reporting helps public health teams understand COVID-19 spread in your area and across the country and informs public health decisions.
POSITIVE RESULT
If the Control (C) line and the Test (T) line are visible, the test is positive. Any faint visible pink/purple test (T) line with the control line (C) should be read as positive.
You do not need to perform repeated testing if you have a positive result at any time.
A positive test result means that the virus that causes COVID-19 was detected in your sample and it is likely you have COVID-19 and are contagious. Please contact your doctor/primary care physician or your local health authority immediately and adhere to the local guidelines regarding self-isolation. There is a very small chance that this test can give a positive result that is incorrect (a false positive).

NEGATIVE RESULT
To increase the chance that the negative result for COVID-19 is accurate, you should:
- Test again in 48 hours if you have symptoms on the first day of testing.
- Test 2 more times at least 48 hours apart if you do not have symptoms on the first day of testing.
A negative test result indicates that the virus that causes COVID-19 was not detected in your sample. A negative result is presumptive, meaning it is not certain that you do not have COVID-19. You may still have COVID-19 and you may still be contagious. There is a higher chance of false negative results with antigen tests compared to laboratory-based tests, such as PCR. If you test negative and continue to experience COVID-19 like symptoms (e.g., fever, cough, and/or shortness of breath) you should seek follow up care with your healthcare provider.

INVALID RESULT
If a control (C) line is not visible, the test is invalid. Re-test with a new swab and new test device.

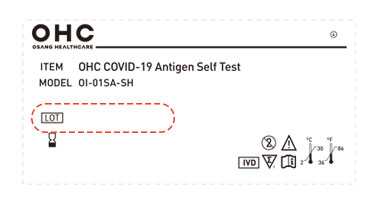
Please check to find out the expiration date by entering the lot number found on your kit
On August 19, 2022, the FDA granted a shelf-life extension for OHC COVID-19 Antigen Self Test
from 8 months to 12 months. To confirm the expiration date, please enter your lot number below.
For the most current expiration dates of this test, please refer to: https://www.fda.gov/covid-test
Enter your lot number :
ABC#####-AB##-###AF
| Lot Number | Printed use by date | Extended use-by date |
|---|---|---|
| Not Found | ||
Where to find your lot number on your test kit
FAQ
Frequently Asked Questions.
-
WHAT IS COVID-19?
COVID-19 is caused by the SARS-CoV-2 virus which is a new virus in humans causing a contagious respiratory illness. COVID-19 can present with mild to severe illness, although some people infected with COVID-19 may have no symptoms at all. Older adults and people of any age who have underlying medical conditions have a higher risk of severe illness from COVID-19. Serious outcomes of COVID-19 include hospitalization and death. The SARS-CoV-2 virus can be spread to others even before a person shows signs or symptoms of being sick (e.g., fever, coughing, difficulty breathing, etc.). A full list of symptoms of COVID-19 can be found at the following link: https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html.
-
WHAT ARE THE KNOWN POTENTIAL RISKS AND BENEFITS OF THIS TEST?
- Potential risks include: - Possible discomfort during sample collection.
- Possible incorrect test result (see Warnings and Result Interpretation sections for more information). - Potential benefits include: - The results, along with other information, can help you and your healthcare provider make informed decisions about your care.
- The results of this test may help limit the spread of COVID-19 to your family and others in your community.
For more information on EUAs go here : https://www.fda.gov/emergency-preparedness-and-response/mcm-legal-regulatory-and-policy-framework/emergency-use-authorization - Potential risks include: - Possible discomfort during sample collection.
-
WILL THIS TEST HURT?
No, the nasal swab is not sharp, and it should not hurt. Sometimes the swab can feel slightly uncomfortable. If you feel pain, please stop the test and seek advice from your healthcare provider.
-
WHAT IS THE DIFFERENCE BETWEEN AN ANTIGEN AND MOLECULAR TEST?
There are different kinds of tests for COVID-19. Molecular tests (also known as PCR tests) detect genetic material from the virus. Antigen tests, such as the OHC COVID-19 Antigen Self Test detect proteins from the virus. Antigen tests are very specific for the COVID-19 virus but are not as sensitive as molecular tests. This means that a positive result is highly accurate, but a negative result does not rule out infection. There is a higher chance of false negative results with antigen tests than with laboratory based molecular tests. This means that there is a higher chance this test will give you a negative result when you have COVID-19. If your test result is negative, you should discuss with your healthcare provider whether an additional molecular test is necessary and if you should continue isolating at home.
-
HOW ACCURATE IS THIS TEST?
The performance of the OHC COVID-19 Antigen Self Test was established in a prospective clinical study using an EUA authorized molecular test as a comparator method (PPA 64.2% and NPA 98.6%). COVID-19 antigen tests are less sensitive than molecular (PCR) tests, and the performance of antigen tests can vary with the amount of COVID-19 protein in your sample. This means that the test may miss as many as 36 cases of COVID-19 out of 100. For more information about the Osang clinical performance, please see the Healthcare provider instructions for use. It is not possible to determine how much virus is in your sample prior to testing and a negative test does not rule out COVID-19 infection. A negative test also does not mean that you are not infectious. You can still have COVID-19 with a negative result from this test and infect other people. For this reason, it is recommended that you test at least twice (serial testing) when using this test. You should contact your healthcare provider to determine if additional testing with a highly sensitive COVID-19 molecular test is recommended. You can find further information by visiting http://www.osanghc.com/en/ifu/hometest. The performance of this test is still being studied in patients without signs and symptoms of respiratory infection and for serial screening. Performance may differ in these populations.
-
WHAT IS SERIAL TESTING?
Serial testing is when one person tests themselves multiple times for COVID-19 on a routine basis, such as every day or every other day. By testing more frequently, you may detect COVID-19 more quickly and reduce spread of infection. Serial testing (i.e. testing every day or every other day) is more likely to detect COVID-19.
Serial testing should be performed in all individuals with negative results; individuals with symptoms of COVID-19 and initial negative results should be tested again after 48 hours. Individuals without symptoms of COVID-19, and with initial negative results, should be tested again after 48 hours and, if the 2nd test is also negative, a 3rd test after an additional 48 hours. You may need to purchase additional tests to perform this serial (repeat) testing.
- If you test negative but continue to have symptoms of COVID-19, and both your first and second tests are negative, you may not have COVID-19, however you should follow-up with your healthcare provider.
- If your test is positive, then proteins from the virus that causes COVID-19 have been found in your sample and you likely have COVID-19
-
WHAT IF YOU TEST POSITIVE?
A positive result means that it is very likely you have COVID-19 because proteins from the virus that causes COVID-19 were found in your sample. You should self isolate from others and contact a healthcare provider for medical advice about your positive result.
-
WHAT IF YOU TEST NEGATIVE?
A negative test result indicates that antigens from the virus that causes COVID-19 were not detected in your sample. However, if you have symptoms of COVID-19, and your first test is negative, you should test again in 48 hours since antigen tests are not as sensitive as molecular tests. If you do not have symptoms and received a negative result, you should test at least two more times with 48 hours in between tests for a total of three tests. If you have a negative result, it does not rule out SARS-CoV-2 infection; you may still be infected and you may still infect others. It is important that you work with your healthcare provider to help you understand the next steps you should take.
-
WHAT DOES AN INVALID TEST MEAN?
An invalid result means the test was not able to tell if you have COVID-19 or not. If the test is invalid, a new swab should be used to collect a new nasal specimen and you should test again with a new test.
Contact Us
- OSANG LLC
- 215 N. Marengo Ave. 3rd Floor
- Pasadena CA 91101
- 844-760-0556
- covidhometest@osangllc.com
Product availability may vary by country.
Distributed by Osang LLC.
Please follow local government and health regulations and guidance with respect to COVID-19 health and safety.
